Thyroid Eye Disease (TED)
With thanks to: Mr Naresh Joshi
Eye problems occur relatively commonly with thyroid disease. TED is also known as Thyroid Associated Ophthalmopathy (TAO) or Grave's Ophthalmopathy. In a small proportion of patients (3-5%) it may be require intensive treatment and can be vision threatening (Fig. 1). Fig.1: Red eyes of thyroid eye disease
Fig.1: Red eyes of thyroid eye disease
Incidence of TED
Eye problems are most commonly associated with Graves’ disease (up to 50% of patients may have signs if examined carefully), but patients with Hashimoto's thyroiditis may also develop problems. In rare cases it can affect patients with primary hypothyroidism and thyroid carcinoma. Those with toxic multinodular goitre, toxic adenoma or diffuse micronodular goitre are usually unaffected.
TED usually occurs in middle age but it may affect any age group from teenagers to those in their 80s (it may even affect newborn babies). Women are much more commonly affected than men, with approximately 4 women affected for every man.
Factors that affect the development of TED include:
- Heredity (30% of patients have a family history of TED and if a twin has TED there is a 1/3-2/3 chance that the other twin will develop problems)
- Stress (this is difficult to define but is thought to play a part in the development of TED)
- Smoking (TED is usually worse in those who smoke cigarettes)
- Environment (because the brother or sister of an affected twin does not always develop TED, as yet unidentified environmental factors must be important)
Causes of Thyroid Eye Disease (TED)
The cause of TED is complex and not fully understood. Almost all patients with Graves' disease have an element of TED, but it does not occur with simple goitres, even though there is over replacement with thyroid hormone. TED can affect people with normally acting thyroid glands (Euthyroid) or even those with under acting thyroid glands (Hypothyroid).
TED may precede thyroid problems in 5-25% of cases, however TED typically occurs about 12-18 months after the development of hyperthyroidism (overactivity of the thyroid gland). It is thought TED is an autoimmune disease occurring along side, but independent of the thyroid disease. Antibodies, like those active against the thyroid, may damage the soft tissues in the orbit (the bony socket of the eye) producing inflammation with enlargement of the muscles and the fat around the eye.
The progress of TED is unpredictable and is often unrelated to the severity of the thyrotoxicosis (hyperthyroidsim). Over all it tends to last 1-3 years with some of the effects being reversible and others, like proptosis, tending to be permanent.
Presentation
There are a wide range of problems and, although some may have serious consequences, the majority are minor, requiring little or no treatment. The problems may be broadly divided into:
- Cosmetic, for example retraction of both the upper and lower eyelids (causing a staring appearance) and protuberant eyeballs (exophthalmos or proptosis) (Fig. 2)
 Fig.2: Upper and lower eyelid retraction of R eye
Fig.2: Upper and lower eyelid retraction of R eye
- Double vision (diplopia) due to limitation of eye movements from inflammation or fibrosis of eye muscles(Fig. 3)
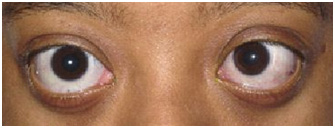 Fig.3: Restriction of eye movements
Fig.3: Restriction of eye movements
- Loss of protection of the front surface of the eye (the cornea) with pain and possibly infection resulting in scarring (which can lead to loss of vision)
- Optic nerve compression (which may lead to loss of vision)
Patients with TED often suffer uncomfortable, red, congested, watery eyes, which may be associated with lid swelling. Retraction of the lids may in part be due to the protuberant eye, but may occur alone due to contraction or over action of the eyelid muscles. This is a relatively common problem and may affect between 32% and 92% of people.
Protuberance (proptosis) of the eyeballs is almost as common. Usually both eyes are involved (although this may be asymmetrical). The cause of protruding eyes is enlargement of the muscles and the fat pushing the eye forward. This may put pressure on the eye causing a rise in eye pressure and the involvement of the eye muscles may prevent the eye moving properly resulting in double vision. Typically this occurs on looking up, and less commonly on left and right gaze.
Loss of protection to the eye surface is usually a combination of proptosis, lid retraction and reduced eye movements. Optic nerve compression is relatively rare, but is an important cause of loss of vision if not treated.
In most cases TED becomes inactive over a period of 3 years. Sometimes it may appear to resolve and then recur before becoming inactive. Problems like eyelid retraction may improve in up to 50% of patients but proptosis and eye movement abnormalities tend to persist.
Investigation of patients with TED
It cannot be emphasised too strongly how important it is that patients with TED see an eye specialist who has a special interest and expertise in the disease. Specific tests are needed in TED in order to fully assess the state of the eyes and the thyroid status. These may include:
- Re-check of thyroid function
- Visual acuity (Checking sight using a vision chart)
- Assessment of eyelid position and function
- Assessment of the eye position within its bony socket, the orbit (exophthalmometry)
- Slit lamp (microscopic) examination of the surface the eye, particularly the cornea
- Pupil testing (a test of optic nerve function)
- Test of eye pressures (intraocular pressure, also known as IOP)
- Colour vision testing (a sensitive test of optic nerve function)
- Examination of the back of the eye, in particular the optic nerve where it enters the eye (this corresponds to the 'blind spot')
- Eye movement assessment (possibly with an orthoptist who specialises in eye movement testing)
- Field of vision test ('a field test', for example with a Humphrey machine)
- CT or MRI of orbits (specialised X-ray or scans to look at the tissues around the eyes)(Fig. 4)
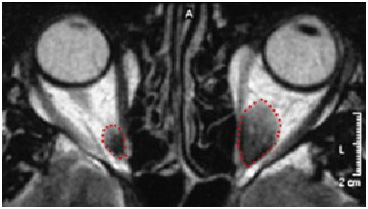 Fig.4: Enlarged L muscles on MRI scan of orbits
Fig.4: Enlarged L muscles on MRI scan of orbits
- Ultrasound scan of the eye muscles
- Visual evoked responses to detect optic nerve damage (rarely used)
Management of mild TED
Local treatments aim to protect the eye and reduce discomfort until TED becomes inactive. Many people suffer dry red irritable eyes because of poor lid movement (sometimes causing a staring appearance) and exposure of the front surface of the eye (due to protuberance of the eyeball). Eyelid swelling and double vision may also be helped by simple measures.
- Simple lubricant eye drops to keep the eye moist during the day
- Ointment in the eye last thing at night if the eye is not closing fully
- If the eyelids do not close fully, protecting the eye at night by taping the eyelids
- Glasses with wide side frames protect the eye from wind and dirt
- Glasses with tinted lenses may also help keep the eyes comfortable
- Guanethidine 2% eye drops are occasionally used for mild staring eyes
- Elevating the head of the bed or using extra pillows can reduce lid swelling that is worse in the mornings
- Double vision can be treated by covering or 'fogging' one side of a pair of glasses. In some cases prisms can be incorporated into glasses or prisms stuck onto the glasses (if double vision is stable) to compensate
- In mild TED with a severe stare, eyelid surgery (for example tarsorrhaphy; ie partially closing the eyelids) under local anaesthetic is effective
Management of severe TED
In severe TED there are two quite distinct problems. The first is management of the acute or active orbital inflammation (usually in the first 12-18 months), which is when vision threatening problems may occur. The second is the chronic or inactive orbital fibrosis (usually after 18 months), particularly affecting the external eye muscles. It is important to realise that all treatments may have undesirable side effects.
Management of Active TED
The following treatments are available:
- High dose steroids
- Other immunosuppressive therapy including 'blood cleaning' (plasma exchange or plasmapheresis)
- Radiotherapy (X-ray treatment) to the eyes
- Surgery to the orbits (decompression)
The most common treatment for severe TED is high dose steroid therapy. The dose regimen varies from centre to centre but steroid treatment is initially given at a high dose and must be gradually reduced (over several weeks) to prevent the disease rebounding (returning). Steroids (oral or intravenous) may be very effective at treating vision threatening optic nerve compression and symptoms due to swelling, but have less effect on proptosis or double vision. However they may be used during the period when surgery is planned for these problems.
Steroids have a wide range of well recognised side effects both in the short and long term. These include: change in facial appearance (Cushingoid facies), weight gain, high blood pressure, increased susceptibility to some infections (for example TB), cataracts, glaucoma, osteoporosis and mental problems. To allow the dose of steroid to be reduced and limit its complications, other immunosuppressive agents may be used in combination with steroid therapy.
Cyclosporin A and Azathioprine are two such agents that are effective in combination and may also be used alone with moderate TED. Units or hospitals with facilities for plasma exchange (which clean the blood, removing the antibodies which are thought to be causing TED) have reported good results with this technique. However, TED may rebound or recur unless immunosuppression is commenced or plasmapheresis is repeated (which is time consuming and not without complications).
Radiotherapy although controversial has been used for many years to treat TED and may be combined with steroids (allowing them to be reduced). It reduces the problems of TED very much like steroids and, while the effects take longer to work, it has the advantage that the improvement is more prolonged. Usually the radiotherapy is given over a period of 2 weeks divided into 10 sessions. The true long-term advantages of radiotherapy are somewhat controversial, but it appears to have good effect on swelling and reduces optic neuropathy (compression). Proptosis and squint, however, are not generally improved. Complications of radiotherapy are rare, particularly with low dose modern treatments. Cataracts, dry eyes and retinal problems are unusual (but may be more likely in diabetics), however, it is recommended that radiotherapy treatment is not repeated because of these risks.
In cases with sight threatening compression of the optic nerve, where medical treatment is not effective, then urgent surgery is necessary. This is called orbital decompression. The orbit (the bony socket that contains the eye) can be thought of as a box or room with an opening in the front, with a roof, a floor and two walls at the sides. These bones are thin and partial removal of one or more creates space for the enlarged muscles and fat surrounding the eye. This removes pressure on the optic nerve and may allow the eye to return to its normal position (also helping protect the front surface of the eye).
There are many methods of orbital decompression, the choice of which depends on the extent of the proptosis (eyeball protuberance); the need to achieve a balanced result and individual surgeons’ preference. Some operations involve an incision on the skin around the eye, others may be made inside the eyelid or it may be possible to operate through the mouth or more commonly via the nose (endoscopic decompression). It may be necessary to combine more than one approach. Surgery is usually performed under general anaesthesia. Complications of surgery include: infection, bleeding, under- or over-correction of proptosis and damage to nerves or eye muscles. Very rarely the vision may be made worse. This surgery is essential when there is significant optic nerve compression with risk of blindness, but it may also be used to treat the cosmetic problem of a prominent eye.
Management of inactive TED
The main problems of inactive TED are double vision (diplopia) , exposure of the surface of the front of the eye and the cosmetic appearance. Until the acute, active situation has settled it is crucial that no surgery is considered (examination stable or unchanged for at least 6 months). The following treatments are available:
Surgery to the eyelids
 Fig.5: Before and after eyelid surgerySurgery to the upper and lower eyelids can improve the patient's appearance and is the most common surgery that TED patients undergo (Fig. 5). It may improve protection of the front surface of the eye as well as give a better cosmetic appearance. Eyelid surgery should take place after strabismus surgery (which should take place after a decompression if planned).
Fig.5: Before and after eyelid surgerySurgery to the upper and lower eyelids can improve the patient's appearance and is the most common surgery that TED patients undergo (Fig. 5). It may improve protection of the front surface of the eye as well as give a better cosmetic appearance. Eyelid surgery should take place after strabismus surgery (which should take place after a decompression if planned).
Tarsorrhaphy (partially closing the eyelids) is simple and like most lid operations can be performed under local anaesthetic. Upper lid retraction may be improved by surgery to weaken or lengthen the muscles that lift the lid. This may involve an incision through the back of the lid or through the skin (hidden in the eyelid skin crease). Lengthening the eyelid muscle may require insertion of some extra tissue as a spacer (not visible from the outside). This tissue is usually taken from other sites where there is excess in the body, for example ear cartilage, inner lining of the mouth (hard palate) or nasal septum.
Improving the lower lid position may require similar surgery. Improvement of the lid position can mask small to moderate degrees of proptosis (prominence of the eyes). Cosmetic surgery (blepharoplasty) can also help the appearance of TED sufferers, particularly by removing the bulges of fat in the upper and lower lid. It is important that bleeding is prevented in this surgery since this may in very rare cases cause visual loss.
Surgery to the external eye muscles (squint surgery)
Double vision may be very disabling and is caused by the external eye muscles becoming fibrosed (scarred). This can be corrected by 'squint-type' surgery (adjusting the eye muscles) and aims to give single vision in a straight-ahead position and in down gaze (for example when reading). It is often not possible to correct diplopia in all positions.
In order to balance the eyes it may be necessary to operate on both eyes even if only one eye appears affected. Sometimes sutures are used that are adjustable to help get the best position for the muscles (the sutures are tied a few hours after surgery with the patient awake). In the majority of cases (up to 80%) it is possible to correct diplopia with one operation, however, others may require several operations over a period of years. Complications of surgery are rare, but it may make the position of the lower lid worse in some cases. Squint surgery should be performed after decompression if one is necessary.
Surgery to the orbit (decompression)
 Fig.6: Before and after orbital decompressionOrbital decompression may be used in inactive TED if the eye is very protuberant causing exposure of the eye surface or poor cosmesis (appearance). It can be very successful at repositioning the eyeball back in its socket (the orbit) (Fig. 6). If an orbital compression is thought necessary, it should be performed before either lid or squint surgery. This surgery is explained along with the treatment of active TED where decompression is used in cases with vision threatening optic nerve compression.
Fig.6: Before and after orbital decompressionOrbital decompression may be used in inactive TED if the eye is very protuberant causing exposure of the eye surface or poor cosmesis (appearance). It can be very successful at repositioning the eyeball back in its socket (the orbit) (Fig. 6). If an orbital compression is thought necessary, it should be performed before either lid or squint surgery. This surgery is explained along with the treatment of active TED where decompression is used in cases with vision threatening optic nerve compression.