Complications of Thyroid Surgery
In expert hands the potential complications of thyroid surgery are all very unusual and low risk, but need to be discussed before operation to allow informed consent for operation. The aim of course is to make the operation as safe as possible, but very occasionally things can go wrong and a complication can occur. These fall into three main areas:
1. Complications of the anaesthetic
Your anaesthetist will discuss with you any possible complications related to the anaesthetic.
2. General complications of any operation
Bleeding
The thyroid gland is surrounded by a number of large and small vessels, especially in patients with thyrotoxicosis. There is a small risk that bleeding can occur in the neck after any form of thyroid surgery, requiring a second operation to stop the bleeding and clear out any clot in the neck. Multiple precautions are taken to minimise the risk of this complication (see webpage Details of Surgery).
 Fig.1: Small postoperative wound seromaIn most cases any bleeding is slow and minor, which may produce a clot (haematoma) or a collection of thin fluid (seroma) under the wound (Fig.1). This occurs in less than 1% of cases. It may be associated with obvious bruising to the skin, but usually requires no treatment as it will resolve by itself with time over about 6 weeks.
Fig.1: Small postoperative wound seromaIn most cases any bleeding is slow and minor, which may produce a clot (haematoma) or a collection of thin fluid (seroma) under the wound (Fig.1). This occurs in less than 1% of cases. It may be associated with obvious bruising to the skin, but usually requires no treatment as it will resolve by itself with time over about 6 weeks.
Occasionally, if the haematoma is large, it will need a minor procedure in outpatients to drain the clot, but no anaesthetic is needed. Although it can look unsightly initially, it is important to note that the long term cosmetic outcome is not affected by these small haematomas.
If you are taking warfarin or clopidogrel these can increase the risk of bleeding in thyroid surgery. Please tell me if you are taking either of them so that I can advise you about stopping these medications prior to the operation. The risk of bleeding if thyroid surgery is undertaken while still on these medications is 10 times higher than the risk of developing a DVT or pulmonary embolus if they are stopped prior to surgery. So all patients need to cease them at an appropriate time before operation; low-dose aspirin (100mg per day) however, can be continued on regardless.
Sudden massive bleeding into the neck is most unusual (less than 1 in 300 patients in our hands) and will usually occur while the patient is in the theatre recovery room or soon afterwards in the ward. 80% of major bleeds occur within the first 6 hours of surgery, and almost all within the first 24 hours, and so it almost never occurs out of hospital. This potential risk of bleeding into the neck is why day case thyroid surgery is avoided and patients are kept in hospital for observation overnight.
Postoperative bleeding it seems is more common in those having had previous surgery, those with large dominant nodules, or a greater extent of surgery, and in those affected by thyrotoxicosis. It is also more common in patients taking anticoagulants (blood thinning drugs). However, none of these are reliable predictors of who might suffer a bleed into the neck after thyroid surgery, meaning that recommending day case thyroid surgery is unsafe.
Treatment in the case of massive bleeding is urgent, as the condition is life-threatening. The neck sutures are immediately removed in the ward, including any deep sutures, to relieve pressure on the trachea, and the patient is returned to theatre to arrest the bleeding and remove the clot.
Pain
This is unusual after minimally invasive surgery as the cut is smaller and I use lots of local anaesthetic in the wound to minimise discomfort after surgery. Generally only paracetamol (Panadol) is needed to control any pain.
Infection & wound scarring
Infection in the wound is extremely rare. Some patients produce very thick scars (hypertrophic or keloid scars); this is more common in black skinned and fair redheaded patients. In patients with generalized eczema, a new area of eczema may develop along the scar.
3. Complications specific to thyroidectomy
Swallowing difficulty
Dysphagia (discomfort with swallowing) is quite common, particularly after a large goitre has been removed, but these symptoms are temporary and will settle with time.
Low calcium levels in the blood
 Fig.2: Tetany due to low calciumHypocalcaemia (low calcium level in the blood) can occur after removal of the thyroid. This is very unusual when only half of the thyroid is removed (as there are two undisturbed glands on the other side) but it is possible. It is quite common after total thyroidectomy, especially for thyrotoxicosis, but this almost always will be a temporary problem.
Fig.2: Tetany due to low calciumHypocalcaemia (low calcium level in the blood) can occur after removal of the thyroid. This is very unusual when only half of the thyroid is removed (as there are two undisturbed glands on the other side) but it is possible. It is quite common after total thyroidectomy, especially for thyrotoxicosis, but this almost always will be a temporary problem.
Hypocalcaemia can occur if the tiny parathyroid glands, which are embedded in the back of the thyroid, are inadvertently damaged or removed. Every effort is made to preserve the parathyroids but they may still not function for a time after the operation.
You may feel tingling or numbness in the fingers or around the mouth, which is an indication that the calcium is low in the blood. In severe cases there may be spasm in the hands or feet , called tetany (Fig. 2), but this is rare. The parathyroids will usually start working normally in a few days to weeks, but meanwhile you may need to take some calcium and vitamin D supplements. I will advise you about how much to take.
These calcium pills (Caltrate Plus) are readily available over the counter at the chemist, and it is worthwhile buying them before surgery so they are on hand at home just in case they are needed after the surgery. There is a 2 in 100 risk of a permanent loss of parathyroid function.
Change in the voice
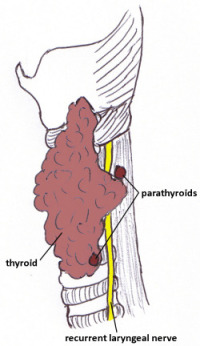 Fig.3: Close relationship of RLN and thyroidVoice change is one of the most dreaded complications of thyroid surgery, but fortunately in expert hands is a rare phenomenon. Patients whose voice is their livelihood should discuss in great detail with their physician the need for thyroidectomy.
Fig.3: Close relationship of RLN and thyroidVoice change is one of the most dreaded complications of thyroid surgery, but fortunately in expert hands is a rare phenomenon. Patients whose voice is their livelihood should discuss in great detail with their physician the need for thyroidectomy.
The nerves to the voicebox run very close to the back of the thyroid on each side of the neck (Fig. 3) and can be damaged or stretched during the operation, especially if the gland is very large or extending into the chest. Damage to the recurrent laryngeal nerve can lead to paralysis of the vocal cord, which can result in a change in the voice. Damage to another nerve (the external branch of the superior laryngeal nerve) can cause difficulty with singing or shouting.
Minor voice changes are not uncommon and are usually transient, lasting for a few weeks. The voice can tire towards the end of the day, and the volume can fluctuate a little in the early days after surgery. Significant hoarseness is usually temporary (4%) but can be permanent in much less than 1% of patients.
Bilateral injury to both recurrent laryngeal nerves is extremely rare, but can result in severe breathing difficulties that will usually require at least a temporary tracheostomy if there is likely to be recovery of at least one nerve, and possibly a permanent tracheostomy.
Further detail about changes to the voice after thyroid surgery can be found on the webpage Thyroid and the Voice.
Low thyroid function
The risk of hypothyroidism (low thyroid state) after thyroid surgery depends on which operation has been performed. In the case of total thyroidectomy all patients will need life-long thyroxine replacement, but in the case of only one lobe being removed (lobectomy) the risk is less than 30%. It is difficult however to predict who will need supplementation after lobectomy, so all patients will need a blood test six to eight weeks after surgery to check the thyroid function. Patients who have had total thyroidectomy will also need this test to check that the replacement dose of thyroid hormone is adequate.
Taking thyroid supplements usually only involves taking one or two small tablets a day, which will be prescribed for you before you leave hospital (see webpage Thyroxine Treatment). The thyroid function is monitored regularly after the operation so that the thyroxine dose can be adjusted if necessary.