Hürthle Cell Tumour
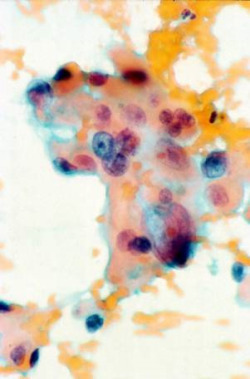 Fig.1: Hurthle cells in FNA cytology specimen showing striking pleomorphism, with very large nuclei, prominent nucleoli and multinucleations.Hürthle cell tumours or neoplasms (HCN) are a distinct subtype of thyroid tumours and are considered a variant of follicular tumours. Although called Hürthle cells, the original cell that Hürthle described was in fact a parafollicular C cell in the thyroid of the dog.
Fig.1: Hurthle cells in FNA cytology specimen showing striking pleomorphism, with very large nuclei, prominent nucleoli and multinucleations.Hürthle cell tumours or neoplasms (HCN) are a distinct subtype of thyroid tumours and are considered a variant of follicular tumours. Although called Hürthle cells, the original cell that Hürthle described was in fact a parafollicular C cell in the thyroid of the dog.
It was the German-Swiss pathologist Askanazy in 1898 who correctly identified the cell that is still known as the Hürthle cell or oncocytic cell.
HCN are encapsulated thyroid tumours that contain more than 75% oncocytic cells, which stain pink under the microscope as they are packed with mitochondria (Fig. 1). The microscopic features can be follicular (most commonly), trabecular, solid or even papillary.
The nuclei of the cells are very pleomorphic and have prominent nucleoli with bizarre isolated forms. The characteristic feature is the distinct granular acidophilic cytoplasm. The cells stain for thyroglobulin, but less so than normal follicular lesions.
Hürthle cells can also be found in a variety of other thyroid conditions such as thyroid irradiation, lymphocytic thyroiditis and Graves' disease.
Presentation & treatment
Most HCN patients present with a solitary thyroid nodule that shows Hürthle cells on FNA cytology, which puts these lesions in the 'suspicious' group (see Thyroid nodules for an explanation of the cytology classification). They are three times more common in women.
One feature that is largely confined to HCN is that FNA cytology may lead to complete infarction (death) of the tumour, probably because of its delicate stroma and increased metabolic oxygen requirements. The lesion occurs particularly in adult women and is usually solid, well vascularised and well encapsulated.
Like non-HCN follicular tumours, the Hürthle cell tumour can be malignant or non-malignant. Of all the Hürthle cell neoplasms, approximately one third will be cancers (HCC). This is more likely in older patients (>55 years), and in those with larger tumours (>4cm).
Because of the increased risk of malignancy in HCN, once the diagnosis is made thyroid surgery is mandatory.
 Fig.2: Hurthle cell adenoma in a thyroid lobectomyIn most cases a thyroid lobectomy is performed to remove the Hürthle cell lesion once diagnosed on cytology (Fig. 2); however total thyroidectomy is generally considered the treatment of choice for Hürthle cell carcinoma. If Hürthle cell carcinoma is diagnosed after hemithyroidectomy on pathology, shown by vascular and/or capsular invasion, then a completion thyroidectomy is performed in a second operation.
Fig.2: Hurthle cell adenoma in a thyroid lobectomyIn most cases a thyroid lobectomy is performed to remove the Hürthle cell lesion once diagnosed on cytology (Fig. 2); however total thyroidectomy is generally considered the treatment of choice for Hürthle cell carcinoma. If Hürthle cell carcinoma is diagnosed after hemithyroidectomy on pathology, shown by vascular and/or capsular invasion, then a completion thyroidectomy is performed in a second operation.
In clinically high-risk cases and in some other situations, a total thyroidectomy may be performed as the first operation. An age >50 years at presentation and a tumour size >4cm carry a higher risk of malignancy and in these patients total thyroidectomy should definitely be considered.
Hürthle cell cancer (HCC)
a) Presentation & Prognosis
Hürthle cell carcinoma has a mean age of presentation between 50 and 60 years, approximately 10 years older than other thyroid cancers. HCC accounts for one third of all HCN, but overall HCC is only found in 3-10% of all thyroid cancers. It is frequently associated with extrathyroidal extension with both lymph node and distant metastases.
These lesions are considered higher risk, but the clinical course is unpredictable and studies have shown widely differing mortality rates. Hürthle cell cancers should be considered more likely to metastasise than follicular cancers. The likelihood of nodal metastases is 10% greater in Hürthle cell tumours than in follicular tumours, but is much less common than with papillary thyroid cancer (PTC). In fact, the prognosis of HCC is probably similar to FTC (follicular thyroid cancer), which is slightly worse than that for PTC (papillary thyroid cancer).
Adverse prognostic factors include older age (>55 years), greater size (>4cm), lymph node and distant metastases, recurrence, and extent of tumour invasion. Controversy exists over the extent of surgery (hemi vs total thyroidectomy) required for these tumours, partly related to the uncertainty of how aggressively the HCC actually behaves.
b) Diagnosis & Surgery
Diagnosis of a malignant HCN relies on the demonstration of capsular and/or vascular invasion at histology, the same criteria used to diagnose malignancy in non-HCN follicular lesions (Figs 3 & 4). Cytology is unable to distinguish benign from malignant tumours.
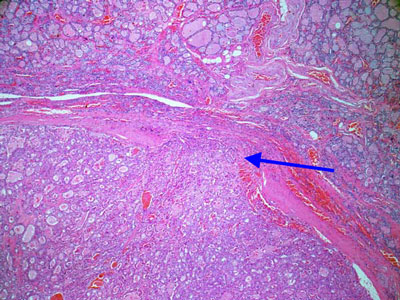 Fig.3: Hurthle cell cancer with capsular invasion (arrow)
Fig.3: Hurthle cell cancer with capsular invasion (arrow)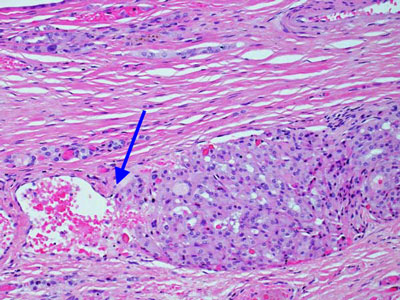 Fig.4: Hurthle cell cancer showing vascular invasion (arrow)
Fig.4: Hurthle cell cancer showing vascular invasion (arrow)
With regards to surgery, most advocate an initial hemithyroidectomy, with completion thyroidectomy if HCC is found on pathology. Because of the frequent lymph node metastases and the fact that nodal involvement is associated with poorer outcome (unlike other well-differentiated thyroid cancers), prophylactic and/or therapeutic neck dissection is indicated as well.
c) Radioactive Iodine
Unlike other follicular lesions, HCC tends not to take up radioactive iodine. Reportedly, approximately 40% of metastases take up radioiodine, compared with 75% of metastases from follicular carcinoma; thus, radioactive iodine treatment, which is the most useful nonsurgical therapy for recurrent well-differentiated thyroid carcinoma, is not always useful in patients with Hürthle cell carcinoma, causing difficulty in treatment for patients who experience recurrences.
Nevertheless, radioactive iodine treatment is used for patients with most of the Hürthle cell cancers after total and near-total thyroidectomy (to destroy any residual thyroid cells) and in the treatment of patients with recurrent and metastatic Hürthle cell carcinoma.
Ablation of any remaining thyroid tissue also facilitates the use of serum thyroglobulin as a tumour marker during followup.
Thyroxine suppression therapy is also indicated, being managed in a similar way to other thyroid cancers, according to the postoperative risk category of the cancer.
NB: I have also created a booklet, outlining the steps in diagnosis and treatment of thyroid cancer, which can be found on webpage Guide to Surgery.