Mr Bill Fleming FRACS, FRCS



I am an Endocrine and General Surgeon at Epworth Freemasons Hospital, and Western Health (Footscray), specialising in endocrine surgery, particularly in minimally invasive thyroid, parathyroid and adrenal surgery. I am the Head of the Western Health Endocrine Surgery Unit, based at Footscray, which is one of the largest units in Melbourne for thyroid, parathyroid and adrenal surgery.
I am a Fellow of the Royal Australasian College of Surgeons (FRACS), a Fellow of the Royal College of Surgeons in England (FRCS), and a Full Member of Australian & New Zealand Endocrine Surgeons (AES).
Endocrine surgeons like me work closely with their medical colleagues (endocrinologists) who are often the doctors who will be responsible for both the initial diagnosis and investigation of endocrine disorders. Endocrinologists may also be involved in long term follow up after endocrine surgery.
I also work in a multidisciplinary team with nuclear medicine physicians, radiologists, pathologists, geneticists and anaesthetists, in order to provide the best care for my patients.
My main private practice is located at Suite 112 in the Freemasons Day Procedure Centre, located at 320 Victoria Parade, East Melbourne (Fig. 1), but I also see patients at my Footscray consulting rooms. I undertake private operations at Epworth Freemasons Hospital in East Melbourne, as well as at the Footscray Hospital.
 Fig.1: My main rooms at Freemasons Day Procedure Centre, East Melbourne
Fig.1: My main rooms at Freemasons Day Procedure Centre, East Melbourne
I trained in Melbourne at the Royal Melbourne Hospital, qualifying in 1982 and gaining the Fellowship of the Royal Australasian College of Surgeons in 1991. I moved to London in 1992 to continue my postgraduate training, specialising in endocrine and pancreatic surgery.
My training in endocrine surgery began at the Kings College Hospital, before I moved to the Hammersmith Hospital, as Senior Registrar to Mr John Lynn and Professor Robin Williamson during 1993 and 1994. I continued my postgraduate training in 1995 as Senior Registrar to Professor Sir Roy Calne at Addenbrookes Hospital in Cambridge, before returning to Melbourne.
In August 1995 I was appointed as a Consultant Surgeon to the Austin Hospital, and Senior Lecturer in the University of Melbourne Department of Surgery, specialising in pancreatic and endocrine surgery. In 2002 I was appointed the Director of General Surgery at the Austin Hospital, responsible for 57 surgeons and junior staff, and helped to establish the Endocrine Surgery Unit. I became a member of the Court of Examiners for the Fellowship of the Royal Australasian College of Surgeons (FRACS) in 2003.
I was invited to return to London as a consultant surgeon in September 2004, commencing practice in endocrine surgery at the Hammersmith (the largest endocrine surgery unit in the UK) and Cromwell Hospitals. I was appointed Honorary Senior Lecturer at Imperial College School of Medicine in 2005, and in the same year was awarded the Fellowship of the Royal College of Surgeons in England. After 4 years in the UK I returned to Melbourne to continue practice in endocrine and general surgery. I was appointed Head of the Endocrine Surgery Unit at Western Health in Footscray in 2011. I was a member of the Court of Examiners for the FRACS from 2010-2019, finishing as the Deputy Senior Examiner.
Surgical Approach
My standard approach for all my endocrine surgical operations is to use minimally invasive surgery. This applies to thyroid and parathyroid operations, as well as to adrenal surgery, where I use laparoscopic (keyhole) techniques. Minimally invasive surgery involves very small incisions, no postoperative drain tubes and often just an overnight stay in hospital.
Day Case Thyroid Surgery
Generally speaking, all forms of thyroid surgery require at least an overnight stay in hospital to monitor and treat any possible complications (particularly bleeding into the neck). Whilst postoperative bleeding into the neck is rare in my hands, if it occurs it can be life-threatening because of acute obstruction of the airway. Immediate removal of the skin sutures may be needed, followed by a rapid return to theatre.
Many studies have shown that if bleeding is going to happen it will almost always occur in the first 24 hours after surgery, and mostly within the first 6 hours. A recent study by the British Association of Endocrine and Thyroid Surgeons (BAETS) showed that although day case thyroidectomy was certainly possible, the risk of catastrophic bleeding taking place at home made it inadvisable. For these reasons I always keep patients in hospital at least overnight after thyroid surgery.
Technical aspects
I use a Ligasure thermal sealing device, a sophisticated new technology which fuses blood vessels and then precisely cuts the sealed vessel. This allows me to avoid the use of any sutures or ties inside the neck (Fig. 2). There is very little pain after the surgery, as I also use plenty of local anaesthetic and most wounds are only 2 or 3cm long.
 Fig.2: ForceTriad generator (left) and Ligasure thermal sealing device (right), which fuses and cuts blood vessels around the thyroid.
Fig.2: ForceTriad generator (left) and Ligasure thermal sealing device (right), which fuses and cuts blood vessels around the thyroid.
All of my patients at the Freemasons and Footscray Hospitals will have their surgery performed with a Medtronic NIM 3.0 intraoperative nerve monitor (Fig. 3), which is used to test and safeguard the recurrent laryngeal nerves (nerves to the voicebox) during your surgery. This nerve monitor minimises the potential risk to the voice to a very low level, and adds an extra level of safety to thyroid and parathyroid operations.
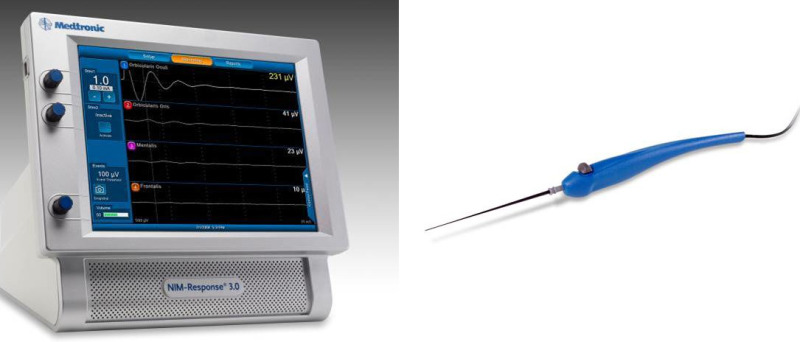 Fig.3: Medtronic NIM intraoperative nerve monitor (left) and the sterile probe used to test the nerve (right)
Fig.3: Medtronic NIM intraoperative nerve monitor (left) and the sterile probe used to test the nerve (right)
My clinical interests are in thyroid, parathyroid and adrenal surgery. I maintain a comprehensive personal database for auditing the outcomes of endocrine surgical procedures, in both public and private practice. I also participate in the Royal Australasian College of Surgeons Continuing Education Program.
My list of publications can be found here.