Preoperative tests
There are a variety of tests that may be performed prior to thyroid surgery in order to plan the best operation for each patient. Most of these are discussed elsewhere on the webpage Thyroid Nodules, but are detailed again here.
Blood tests
Thyroid function can be measured by checking T4 and T3 and TSH. When the thyroid is overactive T3 and T4 are usually high and the TSH is lower than normal. Occasionally T4 is normal, but T3 is raised with a low TSH (T3 thyrotoxicosis). A large prospective study has shown that patients with a high TSH have an 11 times higher incidence of thyroid cancer, probably due to a higher incidence of Hashimoto's thyroiditis in the raised TSH group.
Thyroid antibodies may be checked if there is evidence of thyrotoxicosis or thyroiditis. This may help to predict the need for thyroid replacement following a partial thyroidectomy. Parathyroid function is usually also checked by measuring the calcium and parathyroid hormone (PTH) levels. There is an association of thyroid cancer and parathyroid tumours in patients with a history of neck irradiation.
Imaging
Ultrasound
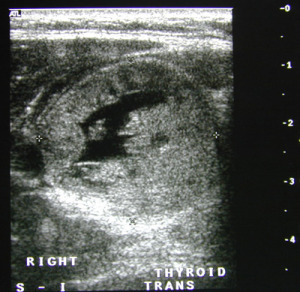 Fig.1: Ultrasound of a thyroid noduleSometimes an ultrasound scan is performed to look at the nodule, although it can throw up more questions than answers at times. More than 20% of patients thought to have a single nodule on examination will have a second nodule on ultrasound, and 10% of patients with a palpable nodule will have nothing found on ultrasound.
Fig.1: Ultrasound of a thyroid noduleSometimes an ultrasound scan is performed to look at the nodule, although it can throw up more questions than answers at times. More than 20% of patients thought to have a single nodule on examination will have a second nodule on ultrasound, and 10% of patients with a palpable nodule will have nothing found on ultrasound.
An ultrasound scan cannot give a definitive answer as to whether a nodule is benign or malignant, but it can show characteristic markings of both and show if the nodule is a cyst. Microcalcifications, irregular borders, marked hypoechogenicity, extraglandular extension, high blood flow and tall shape are all criteria that suggest malignancy (Fig. 1).
Cystic thyroid swellings are less likely to be malignant than solid swellings, but cystic lesions in males are more likely to be malignant than in females. Krukowski's unit in Aberdeen published in 2008 that cysts that recur after aspiration, even with benign (THY2) cytology, should undergo surgery as 54% of patients with benign/non-diagnostic (THY1/2) cytology from recurrent cystic lesions were cancerous.
Nuclear medicine scan
Fig.2: Thyroid scan showing a 'cold' nodule on the left side of the thyroidIf there is evidence of thyrotoxicosis on the thyroid function tests then a nuclear medicine scan, either radioactive iodine or technetium scan, is indicated to discriminate between Graves’ disease, toxic multinodular goitre and a toxic thyroid nodule (Plummer’s disease) (Fig. 2).
Nodules detected by radioactive iodine scans are classified as cold (80%), warm (15%) or hot (5%). If a nodule is not producing thyroid hormones then it will not take up significant amounts of radioactive iodine and will appear 'cold' on the scan. Active nodules appear darker or 'hot' on the scan.
The nuclear medicine scan cannot however distinguish between benign and malignant lesions, but can give a clue as to what is likely. Cold nodules tend to attract more attention because the risk of a thyroid cancer is slightly higher (15%), but thyroid cysts (fluid-filled nodules) and other benign nodules are far more likely (85%).
A nodule that is actively producing hormone will take up the radioactive iodine and appear darker or 'hot' on the scan. Over 95% of all 'hot' nodules are benign, and 90% of 'warm' nodules are benign.
Chest XRay
 Fig.3: Chest XRay with marked tracheal shift to the rightChest XRay may reveal narrowing or displacement of the windpipe (trachea) which is important information for the anaesthetist (Fig. 3).
Fig.3: Chest XRay with marked tracheal shift to the rightChest XRay may reveal narrowing or displacement of the windpipe (trachea) which is important information for the anaesthetist (Fig. 3).
It can also be very useful in showing possible spread of thyroid cancer metastases to the lungs, although CT scan has largely surpassed chest XRay in assessing both of these possible findings.
CT scan
 Fig.4: CT scan with huge goitre narrowing the tracheaThis scan may be performed if there is evidence of airway obstruction like shortness of breath, noisy breathing or voice change, or the goitre appears to be extending behind the breastbone (retrosternal) into the chest.
Fig.4: CT scan with huge goitre narrowing the tracheaThis scan may be performed if there is evidence of airway obstruction like shortness of breath, noisy breathing or voice change, or the goitre appears to be extending behind the breastbone (retrosternal) into the chest.
It is often performed prior to any surgery to assist the anaesthetist in determining if there might be difficulty in placing the endotracheal breathing tube and alerting the surgeon to any potential problems in taking the thyroid out.
CT will show if there is narrowing or displacement of the windpipe (trachea) and how far into the chest that the goitre is growing (Fig. 4).
FNA Cytology
In this test, a very fine needle is inserted into the nodule and a few cells removed for the cytologist to study under a microscope. The cytologist then determines whether the nodule is benign or malignant (see webpage Thyroid Nodules).
Cytology is relatively painless, can be performed with or without local anaesthesia, and ideally should be performed under ultrasound control. A small needle (25-27 gauge) is inserted into the periphery of the nodule and the sample taken. Misdiagnosis of thyroid cysts is possible if FNAC is not performed under ultrasound control. Invariably the fluid contents will give no hint of malignancy, but biopsy of a thickened cyst wall under ultrasound control often identifies thyroid cancer.
The results of thyroid FNA should always be interpreted in the light of the clinical findings and if the cytology does not tally with what has been found on examination then the FNA should be repeated, or consideration given to removing the lump. Clinically suspicious nodules should really be regarded as malignant despite negative cytology, until histological diagnosis has been confirmed.
Cytology may be benign, malignant or non-diagnostic. Accurate diagnoses can be made in colloid nodules and inflammatory thyroid disease (Hashimoto’s, De Quervain’s and tuberculosis). Papillary, medullary, anaplastic cancers and thyroid lymphomas are diagnosed with ease, but the diagnosis of follicular cancers is virtually impossible. If the pathology is bizarre, medullary cancer must be excluded by staining for calcitonin and serum calcitonin analysis. It is best to treat all suspicious cytology surgically.
The classification of the results of fine needle aspiration is complex and can be interpreted as either non-diagnostic, benign, suspicious or malignant. If the FNA is used as a means of separating a benign from a malignant lesion, and no surgery is undertaken, it is essential that the test is repeated within 6 months and, if negative for cancer, again in a year.
In the case of lymphoma of the thyroid, it is usually necessary to do a core biopsy, which is similar to an FNA but uses a larger diameter needle, and is usually carried out under local anaesthetic.
Laryngoscopy
It is valuable for the surgeon to get an independent assessment of vocal cord function preoperatively, and it should ideally be performed if there is a suggestion of voice change, a positive FNA biopsy for cancer, or there has been previous thyroid surgery. The use of voice box assessment is discussed in detail in the webpage Thyroid and the Voice.