Retrosternal (Substernal) Goitre
Presentation
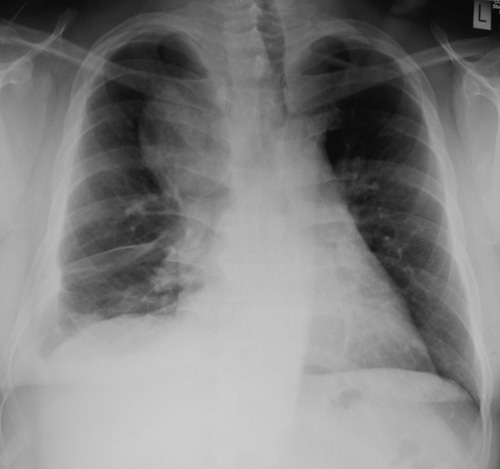 Fig.1: Chest XRay of retrosternal goitre showing marked deviation of the trachea (windpipe) to leftA retrosternal or substernal goitre occurs when the thyroid grows downwards from the neck into the chest. The generally accepted definition is that described by Candela in 2007: any goitre that descends below the plane of the thoracic inlet or grows into the anterior mediastinum for more than 2cm (Fig. 1).
Fig.1: Chest XRay of retrosternal goitre showing marked deviation of the trachea (windpipe) to leftA retrosternal or substernal goitre occurs when the thyroid grows downwards from the neck into the chest. The generally accepted definition is that described by Candela in 2007: any goitre that descends below the plane of the thoracic inlet or grows into the anterior mediastinum for more than 2cm (Fig. 1).
The vast majority of retrosternal goitres are extensions of goitres arising from the neck, but pure intrathoracic goitres do occur, in less than 1%. These isolated goitres remain in the chest, usually entirely asymptomatic and undetected, until the patient has a chest XRay or CT scan.
Retrosternal goitres usually retain some connection from the goitre in the neck, but this may be quite tenuous. They are more likely to be left sided. Very rarely a left sided cervical goitre descends into the right side of the chest, which is called a "crossed substernal goitre".
Retrosternal goitre occurs in 1-15% of all thyroid surgery, and in endemic goitre areas 20% of the population over 70 years old will have a retrosternal goitre.
The natural history of retrosternal goitre is of a slow relentless increase in size, often presenting as an incidental finding on a chest xray in the fifth or sixth decade of life. The most common symptom is a feeling of pressure, because of the limited space at the opening into the chest (thoracic inlet), which leads to the compression of the airway or great veins in the neck. This can give a feeling of breathlessness, or a sensation of congestion in the head, respectively.
 Fig.2: Venous congestion of head and upper chest due to venous obstruction by huge goitrePatients can present with quite marked venous dilatation in the neck and upper chest (Fig. 2), and will often exhibit a positive 'Pemberton's sign' - marked congestion in the face when the arms are raised (Fig. 3).
Fig.2: Venous congestion of head and upper chest due to venous obstruction by huge goitrePatients can present with quite marked venous dilatation in the neck and upper chest (Fig. 2), and will often exhibit a positive 'Pemberton's sign' - marked congestion in the face when the arms are raised (Fig. 3).
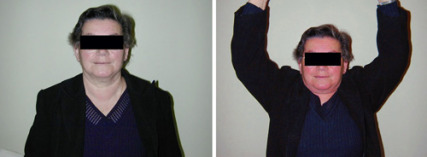 Fig.3: Positive Pemberton's sign indicating obstructionManagement
Fig.3: Positive Pemberton's sign indicating obstructionManagement
Suspected retrosternal goitre should be investigated with CT scan to assess the degree of extension into the chest and to determine the extent and degree of tracheal (windpipe) narrowing and displacement (Fig. 4).
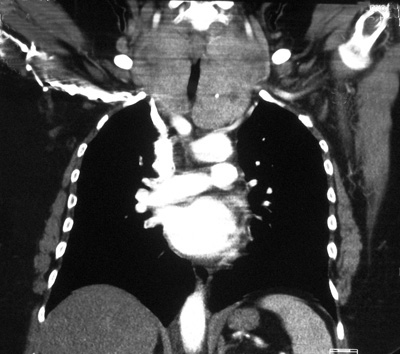 Fig.4: CT scan (of patient in Fig.2) showing huge obstructing goitre narrowing the tracheaThe management of a retrosternal goitre associated with airway obstruction, swallowing problems or major obstruction of arteries or veins is surgical and is not controversial. Any suspicion of malignancy is an absolute indication for surgery.
Fig.4: CT scan (of patient in Fig.2) showing huge obstructing goitre narrowing the tracheaThe management of a retrosternal goitre associated with airway obstruction, swallowing problems or major obstruction of arteries or veins is surgical and is not controversial. Any suspicion of malignancy is an absolute indication for surgery.
The operation of choice is usually a total thyroidectomy, eliminating the need for potential secondary surgery due to regrowth of retained thyroid tissue. Having said that, on many occasions the retrosternal growth is often confined to just one side of the thyroid allowing the possibility of more limited surgery.
The thyroid can almost always be removed through a conventional thyroid incision in the neck, but occasionally division of the upper part of the breast bone (sternum) is necessary, a procedure called a manubriotomy. When this is needed however, it is very well tolerated, usually leaves a thin scar, has minimal complications and produces minimal discomfort (Fig. 5).
 Fig.5: Thin barely visible midline scar of a manubriotomy in the upper chestAsymptomatic retrosternal goitre
Fig.5: Thin barely visible midline scar of a manubriotomy in the upper chestAsymptomatic retrosternal goitre
The term "asymptomatic retrosternal goitre" is actually quite misleading, with an Australian study finding that only 16.6% of retrosternal goitres were asymptomatic. On careful questioning some patients previously diagnosed as having symptoms unrelated to their thyroid do in fact have symptoms that will respond well to thyroidectomy. In the past too much reliance has been placed on the structural impact of the retrosternal goitre and not enough on its physiological effect.
The correct management of asymptomatic retrosternal goitre is unclear and there are two possible approaches: the conservative surgical group argues that the incidence of cancer is no higher than in cervical goitres (a maximum of 3.7 new cases per 1000) and hence in itself not an indication for surgery.
In addition, a study in New York State of over a thousand operations for retrosternal goitre demonstrated a 14-fold increase in mortality compared with that in cervical goitre, and a significantly greater risk of major bleeding and of damage to the parathyroids and recurrent laryngeal nerve.
By contrast the aggressive surgical group feel that all patients with asymptomatic retrosternal goitre who are medically fit should have surgery. They reason that although the risk of cancer is no higher, the diagnosis of any thyroid cancer is compromised by the difficulty of getting a needle biopsy of a goitre that is hidden down in the chest and out of the reach of the surgeon’s clinical examination.
In addition, 5-11% of retrosternal goitres will present at some time with acute airway obstruction and prevention of this dreaded complication is better than an attempted cure. Advancing age is also associated with increased co-morbidities, suggesting that earlier surgery is associated with a reduced risk of complications.
But it is important to note that there are no controlled trials of the management of asymptomatic retrosternal goitre.
Suggested approach to retrosternal goitre
There is no question that patients with significant pressure effects or evidence of thyrotoxicosis or malignancy should be considered for surgery. For ‘asymptomatic’ retrosternal goitre the patient can be reassured that at the moment there is absolutely no evidence to suggest that an uncomplicated retrosternal goitre behaves in any way differently from an uncomplicated goitre in the neck.
However, in fit patients with evidence of airway obstruction or suspicion of malignancy, surgery is indicated and is very safe. If a decision is taken to watch a retrosternal goitre then progressive enlargement on serial CT scans is probably an indication for surgery. The elderly patient with a stable retrosternal goitre can be watched as long as respiratory function is not compromised.
Finally, it is important to emphasise that almost all retrosternal goitres can be removed safely and relatively easily from the chest via a standard thyroid incision in the neck.
Other treatments
Thyroxine treatment in euthyroid (normal thyroid function) patients with large goitres is completely ineffective.
Radioactive iodine is useful and fears of increasing any element of airways obstruction have been allayed by an Australian study in 1997. This demonstrated in large multinodular goitres a subjective improvement in compressive symptoms in 71%, and in 92% a clinically assessed reduction in goitre size after using oral iodine-131 therapy. They used 2.22 GBq (60 mCi) as a cumulative dose over 4 months (555MBq per month). Not all the patients in this study had retrosternal goitres. Previous suggestions that radioactive iodine may precipitate respiratory distress in toxic elderly patients is most likely not valid.
On the other hand, radioactive iodine in most physicians' experience rarely results in a complete resolution of the goitre and is tedious, often needing several doses. It may however, be more beneficial than previously thought, and should therefore be discussed as a possible option in the treatment of retrosternal goitre.