Primary Hyperparathyroidism (PHPT) Symptoms
The symptoms of HPT vary widely from being apparently completely asymptomatic, through vague generalised symptoms, to more severe manifestations and complications of hypercalcaemia.
More than half of all patients with primary HPT have no symptoms or only mild symptoms, and are picked up on biochemical screening for another reason. Despite most patients claiming they feel relatively well at the time of diagnosis, up to 95% notice an improvement in symptoms after parathyroidectomy. Many patients who felt they were asymptomatic preoperatively will claim to sleep better at night, be less fatigued, have less joint and muscle aches, and be able to remember things more easily after their calcium levels return to normal.
Symptomatic presentation due to hypercalcaemia with the classical rhyme of bones, stones, abdominal groans, and psychic moans is extremely rare. However, even today, 4 to 15% of cases will have a history of renal stones. Generally though, the usual symptoms are more vague, such as thirst, lethargy, fatigue, muscle aches and pains and constipation.
Hypercalcaemic crisis, characterised by presentation with a very high serum calcium, occurs in a small number and is an indication for urgent treatment.
Musculoskeletal
The most common symptoms of HPT are muscular weakness, bone and joint pain; fatigue and lethargy are very common. Patients have reduced bone mineral density, but the severe form of bone disease known as osteitis fibrosa cystica (Fig. 1) is extremely rare in developed countries.
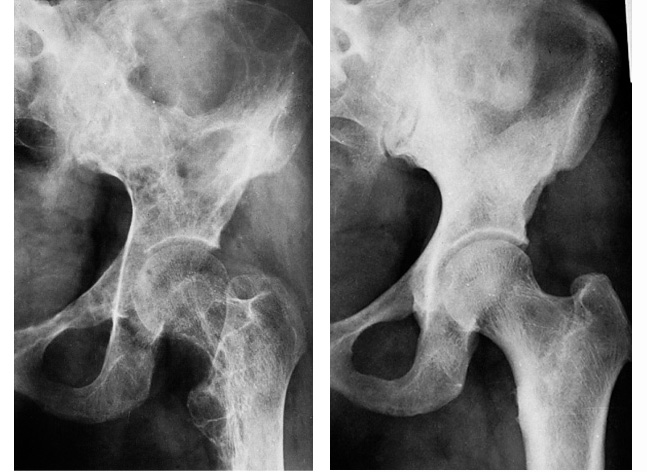 Fig.1: Hip Xray pre and post parathyroidectomy, showing dramatic reduction in bone disease after surgery.
Fig.1: Hip Xray pre and post parathyroidectomy, showing dramatic reduction in bone disease after surgery.
All patients with primary HPT will progressively lose bone density, and even patients with mild asymptomatic pHPT will already have major bone loss at diagnosis. A number of studies have shown that fractures are more common in patients with PHPT.
Parathyroidectomy will increase bone mineral density and reduce the fracture risk, as well as improving muscle function and relieving the feeling of tiredness.
Renal
The kidney is a principal target of PHPT. Renal and ureteric stone disease and nephrocalcinosis (calcium deposits in the kidney) are the most common overt complications of PHPT, but the latter is very rare. Stone disease is multifactorial and is not clearly accounted for on the basis of excessive urinary calcium excretion alone. Parathyroidectomy lowers the frequency of recurrent stones.
The new guidelines for management of asymptomatic patients have a greater emphasis on investigation of potential renal disease caused by PHPT, with measurement of 24 hour urinary calcium, creatinine and creatinine clearance, plus imaging to detect renal stone disease or calcium deposition.
Gastrointestinal
Abdominal pain can arise from chronic constipation, and there is a link between peptic ulceration, pancreatitis and pHPT, although this is controversial. Improvement of symptoms after parathyroidectomy is unpredictable.
Psychological
Prospective analyses have suggested that even apparently asymptomatic patients with pHPT may have neurocognitive / psychiatric symptoms, which may be reversed by active treatment. Anxiety and depression, dementia, loss of concentration or memory are the common symptoms. Parathyroidectomy can reverse the dementia-like symptoms in the elderly population, and significant improvement can occur in other symptoms.
A recent US study showed that sleep disturbances and insomnia are common in patients with pHPT and the majority will gain a significant improvement in their symptoms after parathyroidectomy.
Another study has used a special technique known as single-photon emission computed tomography (SPECT) to look at cerebral blood flow and cerebral metabolism in patients with treated and untreated pHPT. Reduced regional cerebral blood flow has been demonstrated in patients with untreated primary hyperparathyroidism. The results of this study may influence the case for surgical treatment of most cases of pHPT in the future.
Metabolic “syndrome”
Primary HPT is associated with a metabolic syndrome which carries an increased risk of premature death, even in mild hypercalcaemia, and increases with the extent of hypercalcaemia. There is a Swedish study that indicates a possible improvement in survival with parathyroidectomy, but it appears the operation needs to be done early in the disease process to achieve this outcome.
Diabetes mellitus and an impaired glucose tolerance can be seen, due to peripheral insulin resistance. Blood lipid levels show a decrease in HDL and LDL and a rise in VLDL levels. Cardiovascular disorders, such as hypertension, left ventricular hypertrophy and valvular calcification are known to be associated with primary HPT, but the significance is debatable.
Although there is evidence, often subtle, for vascular and cardiovascular dysfunction in some patients with mild PHPT, it is unclear whether these observations are important. At this time, there are no prospective data on cardiovascular outcomes in mild PHPT. Moreover, studies that have tracked cardiovascular endpoints before and after surgery have not shown any benefit when the studies have been rigorously conducted in randomised controlled trials.
A reasonable conclusion to be drawn is that tests for cardiovascular involvement should not currently be part of the workup in PHPT, and that parathyroid surgery should not be performed to improve cardiovascular function, if abnormalities are present.
Many of these effects of the metabolic syndrome can be reversed or improved after parathyroidectomy, but the risk of premature death can persist long after parathyroidectomy, suggesting that there may be irreversible cardiovascular damage in moderate to severe HPT.
Hypercalcaemic crisis
Occurring in either primary or secondary HPT, hypercalcaemic crisis is the presenting feature in 1.6-6.7% of patients with hyperparathyroidism. It is characterised by gastrointestinal symptoms, and marked fatigue, leading to weakness, impaired cognition, cardiac rhythm problems, coma and even death.
The underlying pathology is the same, with adenoma being most likely, but crisis patients tend to have larger gland weights and higher calcium and PTH measurements. Treatment should be fast-tracked, firstly to lower calcium levels, and secondly to localise and remove the causative pathology with urgent surgery.
Following successful surgery, profound hypocalcaemia because of 'bone hunger' can be a problem, particularly if bisphophanates have been used preoperatively to lower calcium levels, requiring careful management.