Parathyroid Cancer
Parathyroid cancers are rare cancers, with only about 1-2 cases per 10,000,000 people per year. They usually occur after middle-age, affecting men and women equally (although men tend to have a worse prognosis) and tend to have a very florid presentation. They are often large and clinically palpable, usually greater than 2 cm in size, and are nearly always functioning tumours. They account for less than 1% of cases of primary hyperparathyroidism.
They also need to be distinguished from atypical parathyroid adenomas, which have no potential to metastasise, but which present with similar symptoms and look very abnormal at surgery.
Presentation
 Fig. 1: Typical neck mass of a parathyroid cancerParathyroid cancers tend to have a very florid presentation, often with the more extreme symptoms of hypercalcaemia like bone disease (90%), with pathological fractures, and renal stones (50-80%), which are much less commonly seen in benign disease. Parathyroid cancers are very symptomatic, with typical features including:
Fig. 1: Typical neck mass of a parathyroid cancerParathyroid cancers tend to have a very florid presentation, often with the more extreme symptoms of hypercalcaemia like bone disease (90%), with pathological fractures, and renal stones (50-80%), which are much less commonly seen in benign disease. Parathyroid cancers are very symptomatic, with typical features including:
- Weakness
- Extreme tiredness and lethargy
- Confusion
- Nausea and vomiting
- Loss of appetite
- Weight loss
- Thirst and polyuria (due to excess calcium being cleared by the kidneys)
- Constipation
- Features of local pressure (or invasion) in the neck, such as dysphagia (difficulty swallowing) or hoarse voice
Examination will often show a palpable neck mass (50% of patients) (Fig. 1), which is almost never found in benign parathyroid disease. In summary, florid symptoms, a palpable mass in the neck, and markedly elevated levels of calcium and PTH, or both, especially in men, should raise the possibility of an underlying parathyroid cancer, although it is important to remember that it is very rare.
Investigation
Measurement of serum calcium and PTH will make the diagnosis of hyperparathyroidism, but will not diagnose cancer itself. The levels of both tend to be very high however, which can suggest the likelihood of cancer.
Imaging studies with Sestamibi scanning usually, but not always, show a very marked hot spot, while ultrasound and CT scanning can show a large mass, usually greater than 2cm in size and separate from the thyroid, or in some cases possibly invading it.
Causes
In most cases the cause of parathyroid cancer is not known, but there is an association with radiation exposure and certain genetic conditions such as Hyperparathyroidism-Jaw Tumour Syndrome (HPT-JT). Mutations of the gene encoding CDC73 (HRPT2, 1q31.2) cause HPT-JT, and a relatively high proportion (approximately 15%) of these patients develop parathyroid cancer. Many sporadic parathyroid carcinomas also exhibit defects in this gene.
HRPT2 encodes a protein called parafibromin, which is thought to act as a tumor suppressor gene. Research has shown that parathyroid carcinomas exhibit loss of parafibromin expression, a fact which can be used to separate atypical adenomas from cancers.
HRPT2 mutations can also be seen in benign parathyroid adenomas, but carcinomas more frequently exhibit alterations in gene copy number and have large-scale chromosomal deletions.
Pathology
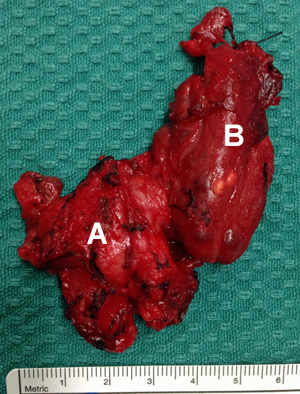 Fig. 2: Parathyroid cancer specimen with cancer (A) and part of thyroid (B) removed together at surgeryThere are two pathologies which can present with very florid symptoms and signs: one is benign (atypical parathyroid adenoma) and the other is malignant (parathyroid cancer).
Fig. 2: Parathyroid cancer specimen with cancer (A) and part of thyroid (B) removed together at surgeryThere are two pathologies which can present with very florid symptoms and signs: one is benign (atypical parathyroid adenoma) and the other is malignant (parathyroid cancer).
Parathyroid cancers (Fig. 2) appear firm, greyish-white, and adherent to adjacent structures, like the thyroid, trachea and neck muscles. Histology of parathyroid cancer (according to WHO criteria) should demonstrate unequivocal invasive growth as evidenced by capsular penetration and definite invasion into adjacent tissue, vascular permeation or perineural spread, or the presence of metastases.
Tumours which show certain clinical, cytological and architectural features which are found in cancer, but lack the features of cancer mentioned above, are called atypical parathyroid adenomas (Fig. 3). These features are extreme hypercalcaemia, adherence to adjacent organs and muscles, solid growth pattern with irregular growth contour, with broad bands of fibrosis.
Unfortunately, these histological criteria are not enough in themselves to confidently make a diagnosis. Parathyroid cancers can be easily confused at the time of operation with atypical adenomas, which do not have the malignant potential to metastasise, but can be very large and sinister looking at parathyroidectomy (Fig. 3).
One way of sorting out potential cancers is to stain the pathology slides for parafibromin, as parathyroid cancers tend to be parafibromin negative.
 Fig. 3: Atypical parathyroid adenoma specimenSummarising, if pathology is benign-looking, and tissue is parafibromin positive, this represents a benign adenoma, while parafibromin negative tissue is likely to represent a low-grade cancer or HPT-JT syndrome.
Fig. 3: Atypical parathyroid adenoma specimenSummarising, if pathology is benign-looking, and tissue is parafibromin positive, this represents a benign adenoma, while parafibromin negative tissue is likely to represent a low-grade cancer or HPT-JT syndrome.
In contrast, if the pathology looks malignant, then parafibromin positivity probably means low-grade cancer, while parafibromin negative tissue is more likely aggressive cancer.
As parafibromin is only involved in 70% of cancers, a further addition to improve diagnostic accuracy has been described. Further staining for Protein Gene Product 9.5 (PGP9.5) can be added to increase specificity. PGP9.5, which is produced by overexpression of UCHL1, has a sensitivity of 78% and 100% specificity, so the combination of both stains together (parafibromin negative and PGP9.5 positive) leads to a confident diagnosis of cancer.
Treatment
The first operation offers the best chance at cure. If the parathyroid tumour is clinically suspicious at operation, with local invasion, large size, or adherence to the thyroid, it should be treated as cancer.
Patients with parathyroid cancer need radical surgery, usually with unilateral clearance of the neck, including hemithyroidectomy en bloc and removal of the local lymph nodes. At all costs, surgery should avoid tumour breach and potential spillage and implantation, which may include sacrifice of the recurrent laryngeal nerve if necessary. There appears to be no value in going back for lymph node clearance if a parathyroid cancer is found unexpectedly at histology, as long as there was no invasion at the time of surgery.
Radiotherapy has no demonstrated benfit, nor has chemotherapy.
Patients have about a 49% 10-year survival, with death usually caused by relentless hypercalcaemia (although this can be controlled well with Cinacalcet medication), rather than local spread of tumour in the neck.