 Hyperparathyroidism in Pregnancy
Hyperparathyroidism in Pregnancy
Implications & Presentation
Hyperparathyroidism can occur during pregnancy, affecting 0.5-1% of pregnant women. It is an indication for urgent investigation and treatment. Untreated HPT is associated with a miscarriage rate 3.5x higher than normal, and many women diagnosed with primary hyperparathyroidism have had previous miscarriages.
There is a strong correlation between the level of serum calcium and the rate of pregnancies lost:
- ca <2.75 - 25% miscarriages
- ca 2.85 - 69%
- ca >3.05 - 80%
Most pregnancies are lost in the late first and early second trimester, which suggests that early investigation and surgery should be undertaken.
During pregnancy, the mother is relatively protected from the rise in serum calcium by the expansion of plasma volume, and active transfer of calcium across the placenta to the foetus. However, foetal intrauterine growth retardation, preterm delivery, permanent hypoparathyroidism and even foetal death can occur. Overall this results in morbidity rates of up to 67% and 80% for mother and foetus, respectively, and infant mortality rates of up to 31%.
The most common complication of elevated serum calcium during pregnancy is renal stones, but pancreatitis is 2-3x more common as well. Most also present with the usual symptoms of excessive tiredness, aches and pains in the bones and joints, etc.
After delivery, maternal calcium levels can rise dangerously because the placental calcium transfer system has been removed. In addition the newborn can develop life-threatening tetany (low calcium in the blood, leading to muscle spasm) because of the suppression of the foetal parathyroid glands in utero.
Investigation
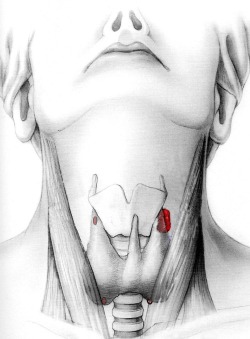
Diagnosis of hyperparathyroidism is usually made on routine biochemical screening, finding an elevated serum calcium. Confirmation of the diagnosis is achieved by measuring serum parathyroid hormone levels (PTH), which are also elevated. The next step would be to localise the parathyroid tumour, but investigation is difficult during pregnancy, as the standard approach of nuclear sestamibi scanning is contraindicated.
Ultrasound should be done however, to try and localise diseased glands and make minimally invasive surgery possible. MRI is also possible as it does not involve ionising radiation, but even successful use of sestamibi nuclear scanning has been reported, when used with lower doses to minimise radiation exposure.
Treatment
Surgical treatment is by far the best option for both mother and foetus, and should be offered as early as possible, although in practice will tend to be in the second trimester. The exceptions to this early surgery rule would be if the diagnosis is made near term, the mother is totally asymptomatic, and the foetus is healthy.
Focused surgery is best if possible, but bilateral neck exploration is often required because of poor localisation, and is usually performed in the second or third trimester. If the patient and foetus can be brought through to term safely, or if the pregnancy is unfortunately lost, surgery should be undertaken post delivery to minimise the risk of future miscarriages.
Medical options are also available to tide the patient over until delivery, such as rehydration, oral phosphate and calcitonin, but bisphosphanates and calcimimetics (e.g. Cinacalcet) are contraindicated, as they will cross the placenta and affect foetal growth.