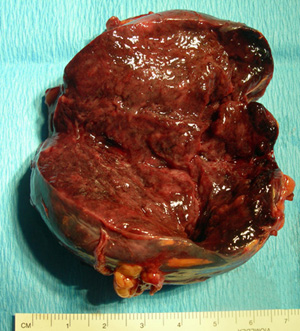
 Fig.1: Operative specimen of a phaeochromocytoma showing the dusky brown colour of its cut surfacePhaeochromocytoma
Fig.1: Operative specimen of a phaeochromocytoma showing the dusky brown colour of its cut surfacePhaeochromocytoma
A phaeochromocytoma is a tumour that arises in the adrenal medulla, from neural crest cells, and secretes catecholamines (Fig. 1). There are approximately 150 new cases diagnosed in Australia each year.
In 1912 the German pathologist Ludwig Pick (Fig. 2) coined the term "phaeochromocytoma" from the Greek 'phaios' (dusky) and 'chromo' (colour).
 Fig.2: Ludwig PickThe phaeochromocytoma is known as the '10 percent tumour' due to a coincidence of 10% probabilities. The tumour normally occurs in only one adrenal but in 10% of cases may arise in both adrenals.
Fig.2: Ludwig PickThe phaeochromocytoma is known as the '10 percent tumour' due to a coincidence of 10% probabilities. The tumour normally occurs in only one adrenal but in 10% of cases may arise in both adrenals.
10% of phaeochromocytomas arise outside the adrenals along the track of the embryological neural crest cells in chromaffin tissue, from the base of the skull all the way down to the scrotum (Fig. 3).
These tumours are known as paragangliomas. In addition 10% of all tumours are malignant, 10% incidentally discovered, and 10% occur in children.
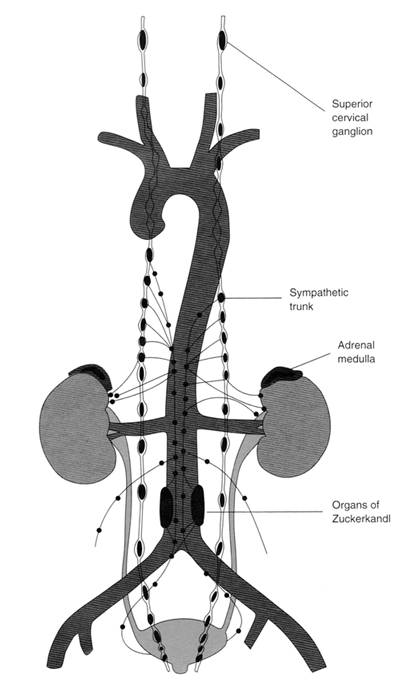 Figure 3: Distribution of chromaffin tissue in the body (from Petri et al, Phaeochromocytomas and symapathetic paragangliomas BJS 2009The catecholamines that may be secreted by a phaeochromocytoma are adrenaline, noradrenaline, dopamine, and L-dihydroxyphenylalanine (L-dopa), but the majority secrete predominantly adrenaline. Although the tumours can also secrete ACTH, serotonin and even parathyroid hormone, most of the symptoms relate to the effects of adrenaline and noradrenaline.
Figure 3: Distribution of chromaffin tissue in the body (from Petri et al, Phaeochromocytomas and symapathetic paragangliomas BJS 2009The catecholamines that may be secreted by a phaeochromocytoma are adrenaline, noradrenaline, dopamine, and L-dihydroxyphenylalanine (L-dopa), but the majority secrete predominantly adrenaline. Although the tumours can also secrete ACTH, serotonin and even parathyroid hormone, most of the symptoms relate to the effects of adrenaline and noradrenaline.
Paragangliomas can be found in locations such as the bladder wall, the thoracic and abdominal paravertebral ganglia and the pericardium of the heart. In children, paragangliomas can be found in the organs of Zuckerkandl.
Paragangliomas lack the enzyme that converts noradrenaline to adrenaline, so typically they secrete only noradrenaline.
The incidence of phaeochromocytoma is very low, accounting for 0.1-0.5% of all cases of hypertension, but it is vital that they are diagnosed as they can be dangerous to the patient and more than 90% are potentially curable.
Typically the tumours can produce marked acute elevations of blood pressure, leading to sudden death. The cause of death in 75% of phaeochromocytoma patients is heart attack or stroke, and one third can die suddenly during or after unrelated minor operations.
Cause of phaeochromocytoma
Sporadic cases typically occur during the fourth and fifth decades of life. In childhood it occurs twice as commonly in males, but in adulthood there is a higher incidence in females.
The exact aetiology of phaeochromocytomas is not well understood, but increasingly the part that genetic factors play are becoming more apparent with further research.
Phaeochromocytomas were originally thought to be familial in 10% of cases (continuing the convenient '10% theme', but over the past decade it has been found that up to 30% of phaeochromocytomas and paragangliomas are related to hereditary tumour syndromes. These include Multiple Endocrine Neoplasia (MEN) types 2A and 2B, von Hippel-Lindau disease (VHL), Neurofibromatosis type 1 (NF1) and the familial paraganglioma syndromes (PGL).
Familial syndromes associated with phaeochromocytomas
There are a number of syndromes associated with phaeochromocytomas and paragangliomas (extra-adrenal tumours). These are:
- multiple endocrine neoplasia type 2 (MEN 2)
- von Hippel-Lindau disease
- neurofibromatosis
- paraganglioma (PGL) syndromes
Multiple endocrine neoplasia type 2 (MEN 2)
This consists of two types, 2A and 2B, due to a mutation in the RET proto-oncogene, and describes the occurrence of a number of tumours in some endocrine glands. Further information can be found on the webpage for MEN 2.
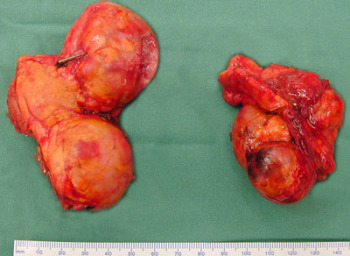 Fig.3: Bilateral phaeochromocytoma specimens from an MEN 2A patientMEN 2A consists of:
Fig.3: Bilateral phaeochromocytoma specimens from an MEN 2A patientMEN 2A consists of:
- medullary thyroid carcinoma
- phaeochromocytoma
- tumours of the parathyroids
MEN 2B consists of:
- medullary thyroid carcinoma
- phaeochromocytoma
- ganglioneuromatosis
- mucosal neuromas on lips and tongue
- Marfanoid habitus
Up to 50% of those with MEN 2 develop phaeochromocytoma, and it is equally common in types 2A and 2B. The tumours are multicentric (diffusely spread in the medulla) and 50-80% are bilateral (Fig. 3). Malignancy is rare and is estimated to be between 0 and 8%. Phaeochromocytomas are usually detected in their early stages in MEN 2 as affected families undergo screening for disease.
Von Hippel-Lindau disease (VHL)
This is an autosomal dominant genetic disease that is characterised by haemangioblastomas in the retina and central nervous system (CNS), especially the cerebellum, and renal cancers. The incidence of phaeochromocytoma in von Hippel-Lindau (VHL) disease is up to 25%. Bilateral phaeochromocytomas occur in 30-40% of patients with VHL and phaeochromocytoma, and malignancy occurs in up to 50%.
VHL is classified as type 1, having the usual tumours of the eye and CNS, without phaeochromocytoma, and type 2A and 2B with the usual tumours plus phaeochromocytoma. There is a further type 2C, which has phaeochromocytoma only.
Other important components of VHL are renal clear cell carcinoma, multiple pancreatic cysts and islet cell carcinoma.
Screening programmes for those with VHL should detect phaeochromocytomas before symptoms occur, although this is complicated by VHL patients being susceptible to a number of adrenal diseases, including cortical adenomas and haemangioblastomas. The accurate diagnostic methods used for phaeochromocytomas will address this difficulty.
Neurofibromatosis type 1 (NF1)
This autosomal dominantly inherited genetic disease is also known as von Recklinghausen disease. It occurs in <5% of all patients with a phaeochromocytoma; about 10% are bilateral and 10% malignant, similar to the general population.
Affected individuals will all eventually develop café-au-lait spots, iris Lisch nodules and multiple neurofibromas. Neurofibromas in patients may secrete noradrenaline with or without a phaeochromocytoma.
Paraganglioma (PGL) syndromes - SDH mutations
PGL syndromes have been genetically characterized as PGL 1, 3 and 4 and are caused by mutations in the succinate dehydrogenase (SDH) subunit D, C and B genes, respectively (SDHD, SDHC and SDHB). Only 10 families worldwide have been described with SDHC mutations, making PGL 3 extremely rare.
Paraganglioma syndromes include predisposition to paraganglial tumours in any location, whereas PGL 1 (SDHD mutation) and 3 (SDHC) patients mostly show only head and neck and upper thorax paragangliomas, which are rarely malignant. All syndromes associated with paraganglial tumours are autosomal dominantly transmitted, but patients with SDHD mutations develop tumours only if they inherit the mutation from the father ('paternal imprinting').
Familial paraganglial tumours are characterized by younger age at diagnosis and more frequently multifocal and extra-adrenal abdominal phaeochromocytomas.
SDHB Mutation
This is the most common of the SDH mutations. 5% of patients will have paragangliomas, 20% phaeochromocytomas (i.e. in adrenal), and 22% have head and neck paragangliomas. 30% will have malignancy.
Other associated tumors include renal cell cancers and GIST in GI tract, and between 10 and 30% will present with additional head and neck tumours at diagnosis.
Patients with PGL 4 (SDHB mutation) and less frequently VHL, are particularly predisposed to malignant and recurrent phaeochromocytoma, which although capable of occurring anywhere in the sympathetic chain, tend to occur below the diaphragm.
Next page: Symptoms & Diagnosis of phaeochromocytoma